Blogs

How to Treat an Ingrown Toenail

Ingrown toenails happen when the edge of the nail grows into the surrounding skin. This can cause pain, redness, swelling and sometimes infection. Soaking the foot in warm water can help soften the area and reduce discomfort. Gently lifting the nail with a small piece of cotton or dental floss may guide it to grow above the skin. Wearing open-toed or roomy shoes can also ease pressure on the toe. However, trying to cut the nail yourself can make things worse. If home care does not help or the area becomes infected, a podiatrist can safely remove part of the nail. In some cases, a small procedure is done to keep the nail from growing back into the skin. If you have a painful toenail that does not improve, it is suggested you see a podiatrist for diagnosis and appropriate treatment.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact Stephanie Tine, DPM of Flamingo Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Fort Lauderdale, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ingrown Toenails
An ingrown toenail is a nail that has curved downward and grown into the skin. This typically occurs at either the nail borders or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. In most cases, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Why Foot Wounds May Not Heal

Foot wounds that do not heal properly are often a sign of underlying health issues that require medical attention. Poor circulation, commonly seen in conditions like diabetes or peripheral artery disease, can limit the flow of oxygen and nutrients necessary for healing. Infections can also delay recovery by causing ongoing inflammation and tissue damage. Other factors, such as repeated pressure, wearing improper footwear, or unrecognized trauma, can keep wounds from closing. Symptoms that indicate a wound is not healing include persistent redness, swelling, drainage, foul odor, or increasing pain. The appearance of black or dead tissue around the wound edges is another serious warning sign. If you have developed a foot wound that is not healing as it should, it is strongly suggested that you promptly contact a podiatrist who can diagnose the cause, and effectively treat cuts and wounds on the feet.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Stephanie Tine, DPM from Flamingo Foot and Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Fort Lauderdale, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Foot Joint Pain and Other Signs of Rheumatoid Arthritis

Joint pain in the feet is often an early and telling sign of rheumatoid arthritis, or RA, a chronic inflammatory condition that targets the joints. This discomfort usually appears in the toes and midfoot, bringing stiffness, warmth, and sensitivity that can make walking difficult. In many cases, swelling develops around the joints, causing a puffy appearance and restricting movement. Heel pain is another symptom, sometimes linked to inflammation where tendons attach to the bone. Some individuals may also experience skin rashes or redness on the feet, adding to the discomfort. These symptoms often appear together and may affect both feet, reflecting the systemic nature of the condition. If you have any of the above symptoms, it is suggested that you promptly contact a podiatrist who can accurately diagnose RA, and offer effective relief methods.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Stephanie Tine, DPM of Flamingo Foot and Ankle. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in Fort Lauderdale, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis in the Feet
Although rheumatoid arthritis attacks multiple bones and joints throughout the entire body, ninety percent of people who actually develop this condition usually do so in the foot or ankle area. Those who develop this kind of arthritis in the feet usually develop symptoms around the toes and forefeet first, before anywhere else. Rheumatoid arthritis appears to have a genetic component. If it runs in the family, then you will be more likely to develop it as well.
Rheumatoid arthritis is an autoimmune disorder in which the body’s own immune system attacks the lining of the membranes surrounding the joints. This causes inflammation of the membrane lining, and the gradual destruction of the joint’s cartilage and even bone.
Some of the most common symptoms that are associated with RA include pain and swelling of the feet. Stiffness in the feet is also another common symptom that people experience. Those who have RA in the feet usually feel the pain in the ball or sole of their feet. This can get to be very painful at times. A person's joints can even shift and become deformed after a period of time.
In order to properly diagnose RA in the feet it is usually necessary for a doctor or podiatrist to evaluate the area. Your doctor will also question you about your medical history, occupation, etc., to determine whether anything in your lifestyle may have triggered the condition. There are a number of tests that may be performed to help diagnose RA, such as a rheumatoid factor test. There is, however, no one single test that will tell you for sure if you have RA. There are different X-rays that can be taken as well to determine if a person has RA in their feet.
There is a range of treatment options for rheumatoid arthritis. Treatment of RA is usually a lifelong process that includes a variety of methods of treatment and therapy. Your doctor can prescribe special shoes that should help with arch support as well as heel support. A physical therapist can help those with this condition learn exercises which will keep their joints flexible. Surgery may be needed to correct some of the issues with the feet, such as bunions, and hammertoes. Fusion is usually the most successful surgical option for rheumatoid arthritis. However, people need to keep in mind that there are some risks associated with these surgeries.
See Your Foot Specialist Regularly If You Work On Your Feet
What Causes Cracked Heels?

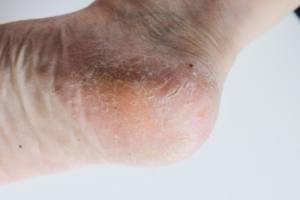
Cracked heels are a common foot condition that can lead to discomfort and even pain if left untreated. They often develop when the skin surrounding the heels becomes dry and thick, leading to splits or fissures. Prolonged standing on hard surfaces can put extra pressure on the feet, causing the skin to expand and crack. As people age, their skin loses moisture and elasticity, making it more prone to dryness. Wearing open-heeled shoes or sandals exposes the heels to air and friction, which can further dry out the skin. Obesity can also contribute to cracked heels, as the increased weight places added pressure on the heel area. Cracked heels can be uncomfortable, and may cause difficulty in completing daily activities. If you have this condition, it is suggested that you confer with a podiatrist who can offer effective treatment solutions, which may include prescribed medication.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Stephanie Tine, DPM from Flamingo Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Fort Lauderdale, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Managing Severe Athlete’s Foot

Severe athlete's foot occurs when the fungal infection extends beyond the toes and affects the entire foot. This condition can cause intense itching, redness, and discomfort, often accompanied by painful blisters called vesicles, or open, pitted sores on the skin. The skin may peel, crack, or become inflamed, making it difficult to walk or wear shoes. The infection can also spread to the toenails or other areas of the foot, leading to a more persistent condition. The cause of severe athlete's foot is a fungal infection that thrives in warm, moist environments. Poor foot hygiene, sweaty socks, tight shoes, and walking barefoot in public places can increase the risk of becoming infected. Symptoms often worsen with movement or activity, causing a burning or stinging sensation. A podiatrist can provide treatment by prescribing antifungal medication or other oral treatments. They may also recommend proper foot care techniques to prevent reinfection and address any complications. If you have severe athlete’s foot, it is suggested that you schedule an appointment with a podiatrist for proper diagnosis and appropriate treatment.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Stephanie Tine, DPM from Flamingo Foot and Ankle. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our office located in Fort Lauderdale, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.