Blogs

Painful Plantar Fasciitis

Plantar fasciitis is perhaps the most common cause of heel pain. It results from inflammation of the thick band of tissue called the plantar fascia, that runs along the bottom of the foot. The primary symptom is sharp, stabbing pain in the heel, particularly when taking your first steps in the morning or after sitting for a while. The pain can lessen with movement but may return after long periods of standing or walking. This condition is often caused by repetitive strain on the plantar fascia, which can be triggered by activities like running, wearing improper footwear, or having flat feet or high arches. A podiatrist can diagnose plantar fasciitis through a physical exam and may use imaging tests for a clearer view. Treatment typically involves stretching exercises, custom orthotics, and anti-inflammatory medication. In more severe cases, corticosteroid injections may be recommended. If you are dealing with this condition, it is suggested that you schedule an appointment with a podiatrist for proper care and relief.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Stephanie Tine, DPM from Flamingo Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Fort Lauderdale, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Facts About Diabetic Neuropathy

Diabetic neuropathy is a common complication of diabetes, causing nerve damage in the feet and legs. Symptoms include numbness, tingling, burning sensations, and sharp or stabbing pain. As nerve function declines, you may lose feeling in your feet, making it harder to detect injuries or pressure points. This lack of sensation can lead to foot ulcers, open sores that often develop on the bottom of the feet. These ulcers can become infected if not treated properly, leading to more serious health issues. A podiatrist plays an essential role in managing diabetic neuropathy and preventing foot ulcers. This type of doctor can assess your feet for signs of nerve damage, provide treatment for ulcers, and recommend appropriate wound care. Additionally, they can help with custom orthotics to reduce pressure on vulnerable areas, and offer advice on proper footwear to prevent further injury. Regular foot exams and monitoring foot health can help catch issues early before they develop into more severe problems. If you have symptoms of this condition, it is suggested that you are under the care of a podiatrist.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Stephanie Tine, DPM from Flamingo Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Fort Lauderdale, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Conditions
According to the American Diabetes Association (ADA), diabetes is a condition that affects approximately 23.6 million Americans. Around 750,000 new cases are diagnosed each year, and the disease’s most common form, Type 2 diabetes, makes up for 90 to 95 percent of these cases. Type 2 diabetes is especially prevalent among older Americans, those who are obese, and those who lead sedentary lifestyles.
Complications of the disease may lead to several foot and ankle-related conditions. The loss of nerve sensation, or neuropathy, can cause diabetics to lose feeling at the bottom of the feet and therefore leave them unaware of pain, pressure, and heat. Decreased circulation is another complication of diabetes that can slow down the healing of wounds and injuries; this can lead to the development of foot ulcers.
To prevent foot ulcers from forming, diabetics should examine their feet every day for small cuts and wear shoes that curtail pressure. Constant monitoring for the risk factors associated with ulcer formation can allow for early detection and therefore lessen the possibility of ulcers or, even worse, amputation. The removal of calluses and ingrown toenails should be left to the podiatrist to avoid improper removal and possible infection.
Diabetic patients may also experience foot deformities due to complications in their feet, such as limited joint mobility, muscle atrophy, and decreased fat padding. These complications can increase pressure in certain areas of the foot, which in turn can cause certain deformities, such as hammertoe, to form. Another deformity, Charcot foot, develops due to the collapsing of microfractures in the bones of the feet. The resulting deformity is a foot that is flattened and wider in appearance.
To help minimize pressure and prevent the development of these diabetes-related foot and ankle conditions, your podiatrist may consider using orthotics or special shoes. Charcot foot may be treated using walkers, custom orthotic insoles, or non-weight-bearing or rigid weight-bearing casts or braces. In more serious cases, surgery may be considered to treat more developed deformities. Ulcers can be further cared for with the help of proper diet, medication to control glucose, intensive wound care, and infection treatment.
Peripheral Neuropathy Occurs When Nerves Stop Communicating Properly

Peripheral neuropathy occurs when nerves outside the brain and spinal cord become damaged, disrupting signals between the brain, spinal cord, and the rest of the body. This can lead to numbness, tingling, burning, or weakness, often starting in the feet. Causes vary but include diabetes, infections, vitamin deficiencies, and prolonged pressure on nerves. People with neuropathy may struggle with balance, coordination, and even simple tasks like walking or sensing temperature changes. Over time, nerve damage can worsen, leading to foot injuries or ulcers that may go unnoticed due to reduced sensation. Treatment focuses on managing the underlying cause, relieving symptoms, and preventing complications. Medications, lifestyle changes, and targeted exercises can help improve nerve function. Proper foot care is essential to avoid further injury. If you are experiencing unexplained foot pain, numbness, or weakness, it is suggested that you see a podiatrist for evaluation and appropriate care.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Stephanie Tine, DPM from Flamingo Foot and Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Fort Lauderdale, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is the weakness, numbness, and pain in the hands and feet due to damage to the peripheral nerves. The peripheral nerves are responsible for sending information from the brain and spinal cord to the rest of your body. Causes of Neuropathy include: traumatic injuries, infections, metabolic problems, exposure to toxins, and diabetes.
Diabetes is the most common cause, with more than half of the diabetic population developing some type of neuropathy. There are several types of neuropathy and they vary based on the damage of the nerves. Mononeuropathy is classified as only one nerve being damaged. When multiple nerves are affected, it is referred as polyneuropathy. One of the types of polyneuropathy is distal symmetric polyneuropathy. It is the most common for people with diabetes and starts when the nerves furthest away from the central nervous begin to malfunction. The symptoms begin with pain and numbness in the feet and then they travel up to the legs. A rarer form of polyneuropathy is acute symmetrical peripheral neuropathy, which is a severe type that affects nerves throughout the body and is highly associated with Guillain-Barre syndrome, an autoimmune disorder that attacks the peripheral nervous system and can be fatal. Although there are many types of neuropathy, most of them share the same symptoms such as pain, extreme sensitivity to touch, lack of coordination, muscle weakness, dizziness, and digestive problems. Since neuropathy affects the nerves, those affected should be careful of burns, infection and falling, as depleted sensations disguise such ailments.
The best way to prevent neuropathy is to manage any medical conditions such as diabetes, alcoholism, or rheumatoid arthritis. Creating and managing a healthy lifestyle can also go a long way. Having a healthy diet full of fruits, vegetables, whole grains and lean protein can keep the nerves healthy. These types of food have the nutrients to prevent neuropathy. Regularly exercising can help as well, but it is best to consult with a doctor about the right amount. In addition to diet and exercise, avoiding risk factors will also prevent neuropathy. This includes repetitive motions, cramped positions, exposure to toxic chemicals, smoking and overindulging on alcohol.
Facts About Tarsal Tunnel Syndrome

Tarsal tunnel syndrome is caused by the compression of the posterior tibial nerve as it passes through the tarsal tunnel, located on the inside of the ankle. This compression can lead to various symptoms such as numbness, tingling, burning sensations, and sharp pain in the foot and ankle area. These symptoms often worsen with prolonged standing, walking, or activity. The causes of tarsal tunnel syndrome include trauma, repetitive stress, or conditions like diabetes that lead to nerve damage. Other contributing factors include swelling, cysts, or flat feet, which can narrow the tunnel and put pressure on the nerve. To diagnose tarsal tunnel syndrome, podiatrists rely on a thorough physical examination and may use imaging tests like MRI scans or ultrasounds to assess the area. Nerve conduction studies may also be performed to measure the electrical activity of the nerves and confirm the diagnosis. If you are experiencing any of the above symptoms, it is suggested that you confer with a podiatrist who can provide an accurate diagnosis and treatment.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Stephanie Tine, DPM of Flamingo Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our office located in Fort Lauderdale, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which the tibial nerve, located in the tarsal tunnel in the foot, is compressed. The tibial nerve can become compressed from injury, such as an ankle sprain, flat feet, and lesions. Arthritis, diabetes, and varicose veins can also cause swelling and thus result in nerve compression.
Symptoms of tarsal tunnel syndrome include several different sensations in the sole of the foot, inside the ankle, and around the tibial nerve. These sensations include shooting pains, numbness or reduced sensation, pins and needles, burning, and tingling. Symptoms tend to worsen with greater activity to the area. In rare and severe occasions, this can change the muscles in the foot.
If you suspect you have tarsal tunnel syndrome, you should consult with your podiatrist. He or she will examine your medical history to see if you have a history of diabetes, arthritis, or flat feet. They will also check to see if you have suffered an injury to the area recently. An electrical test will be conducted to check if the nerve has been damaged. A simpler Tinel’s Test might also be used. This includes simply tapping the nerve to create a sensation. An MRI scan of the area may also be used.
Treatments vary greatly for tarsal tunnel syndrome. Treatments include both nonsurgical and surgical options depending upon the severity of the condition. Nonsurgical options include anti-inflammatory medication and steroid injections to the area. Orthotics, such as a splint or brace that immobilizes the foot, is another noninvasive option. For those with flat feet, custom shoes can be made to offer better foot support. Surgical options include a tunnel tarsal release, in which an incision is made behind the ankle down to the arch of the foot. This releases the ligament and relieves pressure off the nerve. Some doctors use a more minimally invasive surgery, where smaller incisions are made in the ankle and the ligament is stretched out.
If you are suffering from painful sensations in your foot, see a podiatrist who can determine if you are experiencing tarsal tunnel syndrome. Tarsal tunnel syndrome that is left unchecked can cause permanent nerve damage to the foot.
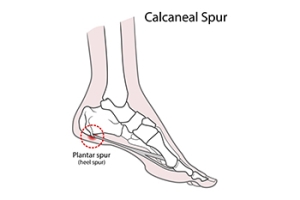
Symptoms and Risk Factors of Heel Spurs
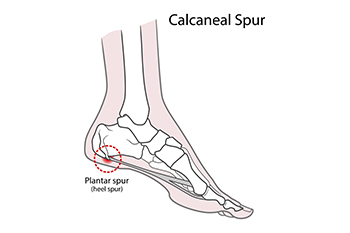
A heel spur is a bony growth that forms on the underside of the heel bone, often caused by long-term strain on the foot’s ligaments and muscles. This condition usually develops as a result of repetitive stress, such as excessive walking or running, which can lead to inflammation and the formation of calcium deposits. The primary symptom of a heel spur is sharp pain, especially when standing or walking after long periods of rest. The pain may decrease as the foot warms up, but it can return with prolonged activity. Risk factors for developing a heel spur include having flat feet, being overweight, wearing poorly fitting shoes, or engaging in activities that put excessive pressure on the feet, like running on hard surfaces. Additionally, people with conditions like arthritis or diabetes may also be at a higher risk. If you have heel pain, it is suggested that you consult a podiatrist who can provide an accurate diagnosis and appropriate treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Stephanie Tine, DPM from Flamingo Foot and Ankle. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Fort Lauderdale, FL . We offer the latest in diagnostic and treatment technology to meet your needs.